Abstract
Recent international consensus guidelines recommend that patients with significant bleeding phenotypes and plasma VWF levels in the 30-50 IU/dL range should be classified as Low von Willebrand factor (Low VWF). Critically however, evidence-based guidelines regarding optimal clinical management strategies for this cohort have not been defined. In particular, data regarding the need for hemostatic cover for procedures in Low VWF are limited. To address this deficit, as part of the Low Von Willebrand in Ireland Cohort (LoVIC) study we conducted a systematic retrospective review of all procedures in a large cohort of well characterised patients with Low VWF.
Methods:
Following written informed consent, we collated data on all procedures performed in LoVIC patients over a 17 year period (1/1/00-12/31/17). Case notes were reviewed and data collected in a standard proforma - age at intervention, choice of hemostatic cover, perioperative VWF, haemoglobin (Hgb) levels and reported bleeding. Procedures were categorised as dental extractions (DE), minor (e.g. endoscopies, joint injections) or major surgery. Tranexamic acid (TA) was prescribed 1g TDS. All desmopressin (DDAVP) was administered intravenously (IV, 0.3mg/kg).
Results:
165 procedures in 65 LoVIC participants were identified. The procedural group was significantly older (median 45 vs 38.8 years, p<0.0001) and with a longer duration of Low VWF (9.0 vs 6.5 years, p=0.02) compared to the rest of the cohort. The majority of procedures were either minor (69.1%) or DEs (24.2%), with only 11 major procedures. Overall, 41 (24.8%) were covered with TA alone; 103 (62.4%) with DDAVP+/- TA; clotting factor concentrate (CFC) was used in only 4 procedures.
Dental extractions:
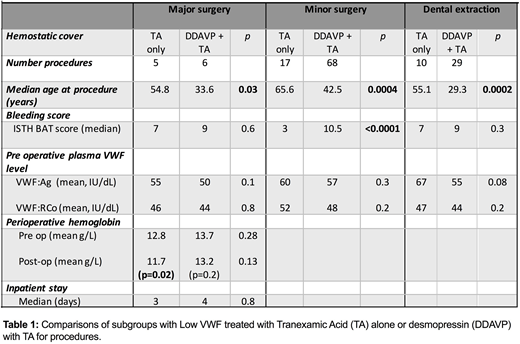
DDAVP+/-TA was used in 72.5% of DEs with no excess bleeding. Of the 10 DE with only TA, 4 developed bleeding requiring treatment (DDAVP/suturing/TA). On comparison of the DDAVP/TA and TA groups, no significant difference in ISTH BAT (median 9 vs 7, p=0.3) or plasma VWF levels (Table 1) at time of procedure was seen. However, the TA only cohort were significantly older (median 55.1 vs 29.3 years, y, p=0.0002), influencing treatment choice. Of interest, in the 4/10 with TA only who bled, pre-DE plasma VWF levels were close to or within the normal range (VWF:RCo 47- 79 IU/dL).
Minor procedures:
Of the 114 minor procedures, 45.6% (52) were endoscopies, 31 with biopsy. The other 62 procedures were dermatological (19), orthopaedic (19), gynecological (8) or other (e.g. minor biopsies, 14). 17 procedures with low bleeding risk were performed with no hemostatic cover independent of the coagulation service. Excessive bruising was reported in 2/17 procedures, both patients were older (54 and 70 years) with pre-op plasma VWF levels within the normal range.
For the remaining 97 procedures, 3 patients had CFC cover (unsuitable for DDAVP); 68 DDAVP/TA and 26 received only TA. Age contributed to prophylaxis choice, with TA cohort significantly older than the DDAVP/TA group (median 65.6 vs 42.5y, p=0.0004). However, phenotype also influenced with ISTH BAT scores significantly lower in the TA only cohort (median 3 vs 10.5, p<0.0001). No bleeding or significant change in perioperative Hgb levels were reported in any procedure covered with prophylaxis.
Major :
Data on major procedures were limited to 11 procedures covered with TA or DDAVP/TA. Plasma VWF levels were maintained following a single dose of DDAVP in all cases. A significant reduction in post-op Hgb levels was observed in TA only patients but no significant bleeding occurred (Table 1). The TA group were significantly older than DDAVP/TA patients (54.8 vs 33.6,p=0.03) but no significant difference in ISTH BAT score, pre-operative plasma VWF or Hgb levels or inpatient stay was seen, although numbers are limited.
Conclusion:
This study represents the largest analysis of procedural outcomes in patients with Low VWF to date. Our data suggest that age and ISTH BAT score significantly influence choice of hemostatic prophylaxis. Bleeding complications were observed only in LoVIC patients undergoing DE covered by TA, or with minor procedures with no hemostatic cover. Interestingly, patients who developed bleeding were typically older (median 59.7y) and, critically in this subgroup, bleeding occurred despite that plasma VWF levels had corrected to within the normal range, clearly raising the possibility that age-corrected normal ranges may need to be considered.
Lavin:Shire: Honoraria, Research Funding, Speakers Bureau. O'Donnell:Bayer: Research Funding, Speakers Bureau; Baxter: Research Funding, Speakers Bureau; Shire: Research Funding, Speakers Bureau; Novo Nordisk: Research Funding, Speakers Bureau; Leo Pharma: Speakers Bureau; Octapharma: Speakers Bureau; CSL Behring: Consultancy; Daiichi Sankyo: Consultancy; Pfizer: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal